World Pancreatic
Cancer Day
16 November 2023
On World Pancreatic Cancer Day, at DiCE we raise awareness of pancreatic cancer, the symptoms, and risk factors, and the urgent need for earlier detection and new research. We need to take action to increase the five-year survival rate of this deadly disease.
The time to act is now.
Facts
Pancreatic cancer is the fourth most common cause of cancer deaths in the EU, it has the lowest rate of survival amongst all cancers across Europe killing about 92% of patients within 5 years of their diagnosis1. In 2018 it took the lives of approximately 128 000 Europeans, while another 132 600 were diagnosed2.
It ranks second – after colon cancer -– in incidence and costs among digestive cancers, with the total costs reaching €7 billion in Europe. One of the major reasons why pancreatic cancer is associated with such poor outcomes is because it is usually diagnosed at a late stage, 80% of patients already have tumors that are diagnosed in a stage when it is too late to be cured. The 5-year survival rate for pancreatic cancer is 9%.
Investment in research for effective targeted therapies and data collection is lacking.
1. Minicozzi P, Cassetti T, Vener C, et al.. Analysis of incidence, mortality and survival for pancreatic and biliary tract cancers across Europe, with assessment of influence of revised European age standardisation on estimates. Cancer Epidemiol 2018;55:52–60. 10.1016/j.canep.2018.04.01
2. Ferlay J, Colombet M, Soerjomataram I, et al.. Cancer incidence and mortality patterns in Europe: estimates for 40 countries and 25 major cancers in 2018. Eur J Cancer 2018;103:356–87. 10.1016/j.ejca.2018.07.005
Raise awareness
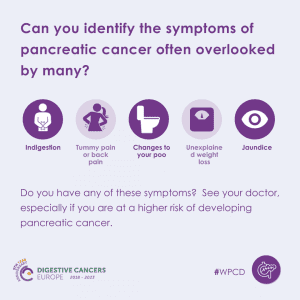
It is critical to raise awareness about pancreatic cancer, the symptoms and risks of this disease, and the urgent need for earlier detection.
With a five-year survival rate, pancreatic cancer is one of the world’s deadliest cancers. One of the reasons for this low survival rate is a general lack of knowledge about the pancreas. It’s pivotal to know the symptoms and risks of this disease. Unlike other cancers, doctors have no simple way of spotting pancreatic cancer. No blood test, no screening, no simple test.
The importance of early diagnosis
Pancreatic cancer is particularly hard to diagnose. Signs and symptoms can often be vague and non-specific, so misdiagnosis is very common, resulting in many patients not being diagnosed until their cancer is at an advanced stage. At this late stage, surgery is usually not possible – the only treatment that has the potential to cure the disease. More than half of people diagnosed with pancreatic cancer die within 3 months. For long-term survival of pancreatic cancer, early detection is critical as it opens the door to the best option for a positive outcome – surgery.
A simple way to diagnose people earlier and save lives from pancreatic cancer is paramount.
Risk factors
Older age is the strongest risk factor; incidence peaks at 65-69 years in males and 75-79 years in females1,2. Most pancreatic cancers (>80%) arise due to sporadically occurring somatic mutations. Only a small percentage is due to inherited mutations3, (the most common genetic mutations are variants in BRCA2. Those from families at risk should receive genetic counselling and be considered for enrolment in investigational screening registries. Currently, the procedures for surveillance Individuals are annual endoscopic ultrasound (EUS) and/or pancreatic magnetic resonance imaging (MRI)4. Surveillance data in high-risk individuals demonstrated high rates of resectability and encouraging observations of long-term survival1, 5-9.
In sporadic pancreatic cancer, the main risk factors are tobacco, Helicobacter pylori infection and dietary habits (i.e., high red meat, high alcohol intake, low fruit and vegetable intake), overweight/obesity and type 2 diabetes mellitus)1,2,10,11. Chronic pancreatitis is also a risk factor for PC.
References
- Conroy, T. et al. Pancreatic cancer: ESMO Clinical Practice Guideline for diagnosis, treatment and follow-up. Annals of Oncology.
- GBD 2017 Pancreatic Cancer Collaborators. The global, regional, and national burden of pancreatic cancer and its attributable risk factors in 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet Gastroenterol Hepatol. 2019;4(12):934-947.
- Pereira SP, Oldfield L, Ney A et al. Early detection of pancreatic cancer. Lancet Gastroenterol Hepatol. 2020;5(7):698-710.
- Stjepanovic N, Moreira L, Carneiro F et al. Hereditary gastrointestinal cancers: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2019;30(10):1558-1571.
- Owens DK, Davidson KW, Krist AH et al. Screening for Pancreatic Cancer. JAMA. 2019;322(5):438.
- Yurgelun MB. Building on More Than 20 Years of Progress in Pancreatic Cancer Surveillance for High-Risk Individuals. J Clin Oncol.2022;40(28):3230-3234.
- Klatte DCF, Boekestijn B, Wasser M et al. Pancreatic Cancer Surveillance in Carriers of a Germline CDKN2A Pathogenic Variant: Yield and Outcomes of a20-Year Prospective Follow-Up. J Clin Oncol. 2022;40(28):3267-3277.
- Dbouk M, Katona BW, Brand RE et al. The Multicenter Cancer of Pancreas Screening Study: Impact on Stage and Survival. J Clin Oncol.2022;40(28):3257-3266.
- Sawhney MS, Calderwood AH, Thosani NC et al. ASGE guideline on screening for pancreatic cancer in individuals with genetic susceptibility: summary and recommendations. Gastrointest Endosc. 2022;95(5):817-826.
- Maisonneuve P, Lowenfels AB. Risk factors for pancreatic cancer: a summary review of meta-analytical studies. Int J Epidemiol. 2015;44(1):186-198.
- Yu J, Yang X, He W et al. Burden of pancreatic cancer along with attributable risk factors in Europe between 1990 and 2019, and projections until 2039. Int J Cancer. 2021;149(5):993-1001