Colorectal Cancer (Bowel Cancer) Treatments
Surgery
Surgery
Surgery is often the main treatment for earlier-stage colorectal cancers. The type of surgery carried out depends on the stage (extent) of the cancer, where it is, and the goal of the surgery.
Types of surgery for colorectal cancer
Removal of polyps (polypectomy) and local excision
- Some early colorectal cancers (stage T0is and some early stage I tumours) and most polyps can be removed during a colonoscopy. The procedure is called a polypectomy. It is usually done by passing a wire loop through the colonoscope to cut the polyp off the wall of the colon with an electric current. The procedure is painless.
- A local excision (cutting out tissue) is a slightly different procedure. Tools are used through the colonoscope to remove small cancer lesions on the inside lining of the colon along with a small amount of surrounding healthy tissue on the wall of colon.
Removal of part of the colon (colectomy)
- Tumours that cannot be removed with local excision will need more extended surgery.
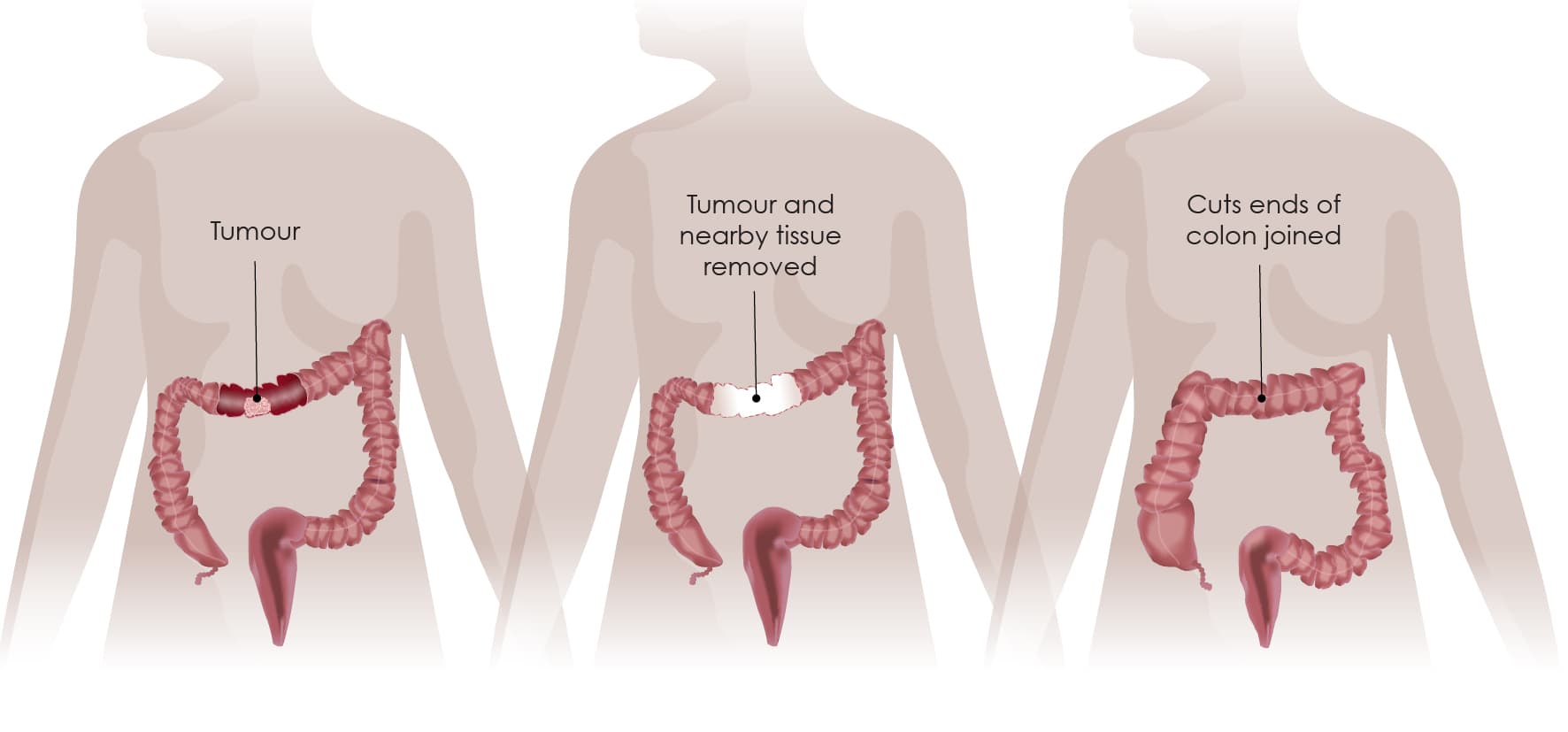
- A surgeon will remove a part of the colon (partial resection), also called a colectomy, or hemicolectomy, removing the cancer and a small amount of healthy tissue around it. The two ends of the remaining colon are sewn or stapled back together – this is called anastomosis.
An illustration of a colectomy with anastomosis. The first image (left panel) shows the colon with the tumour. The second image (middle panel) shows the colon during surgery – the tumour has been removed, while the two parts of the colon are not joined together yet. The third image (right panel) shows the two previously cut parts of the colon joined.
- Depending on the location of the tumour these resections are called something different:
- If the tumour is located in the right side of the colon-the ascending colon-this is called a right hemicolectomy.
- If the tumour is located in the left side of the colon-the descending colon-this is called a left hemicolectomy.
- If the tumour is located in the sigmoid colon-this is called a sigmoid resection.
- Right and left hemicolectomies are sometimes extended to the transverse colon and are then called extended (right or left) hemicolectomy.
For these procedures, abdominal surgery is required. This can be done in two ways:
- Open surgery (laparotomy)
- This procedure is done through a single long incision (cut) in the abdomen.
- Keyhole surgery (laparoscopy)
- This procedure is done through many smaller incisions (cuts) and with special tools. A laparoscope is a long, thin tube with a small camera and light on the end that lets the surgeon see inside the abdomen. It is placed into one of the small cuts, and long, thin instruments are put in through the others to perform the surgery.
- Because the incisions are smaller in a laparoscopic-assisted surgery than in a laparotomy, patients often recover faster and may be able to leave the hospital sooner than they would after an open surgery. However, this type of surgery requires special expertise, and it might not be the best approach for everyone.
Colostomies & stomas
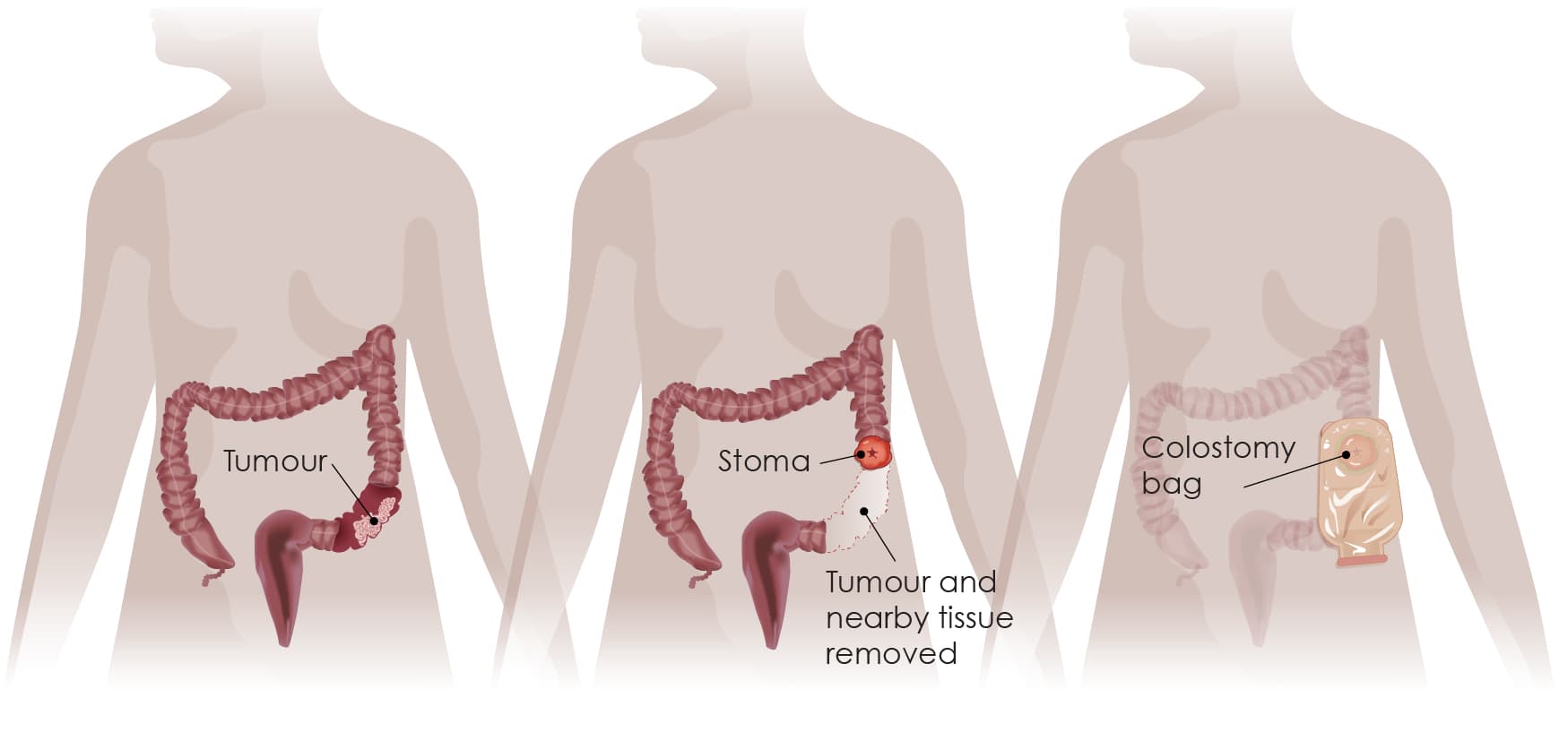
A colostomy is a procedure that creates an opening (a stoma) for the colon, or large intestine, through the abdomen.
This part of the intestine then empties into a bag, known as a stoma bag, which is stuck onto your skin. The stoma bag is a small waterproof pouch used to collect your bowel waste (stools). You will need to regularly empty and change this bag. How often it needs to be changed depends on which type of bag you use, but it may need changing around one to three times a day.
An illustration of colon cancer surgery with colostomy. The first image (left panel) shows the colon with the tumour. The second image (middle panel) shows the colon during surgery – the tumour has been removed, while the two parts of the colon are not joined together yet; a stoma has been created. The third image (right panel) shows a colostomy or stoma bag attached to the stoma.
A stoma may be temporary or permanent. It is often a temporary solution for a few months to allow your colon time to heal after surgery. Then a second operation, known as anastomosis, is performed to join the two ends of the colon together and close the stoma. Some people may need a permanent stoma, for example if the remaining ends of the colon or those between the colon and the rectum cannot be joined together.
These days, bags and pouches are very discreet, and contain special filters to prevent any unpleasant smells. But it might take some getting used to. Your doctor or nurse will be able to provide you with all the information and guidance you need to help you become accustomed to a stoma.
Types of surgery for rectal cancer
There are some surgical procedures that are specific to rectal cancer.
- Transanal excision (TAE)
- This procedure can be used to remove some early stage I rectal cancers that are relatively small and not too far from the anus. The surgeon performs surgery directly through the anus and removes the rectal tumours and small amounts of surrounding tissue while leaving the anus and sphincter – the muscle that keeps the anus closed and prevents stool leakage – intact.
- Transanal endoscopic microsurgery (TEM)
- This procedure can be used for early stage I cancers that are located higher in the rectum and cannot be reached using transanal excision (TAE). Guided by a video monitor, the surgeon utilises special equipment, through the anal canal to remove the tumour and lymph nodes.
Because both TAE and TEM do not involve cutting open the abdomen the healing time is much shorter.
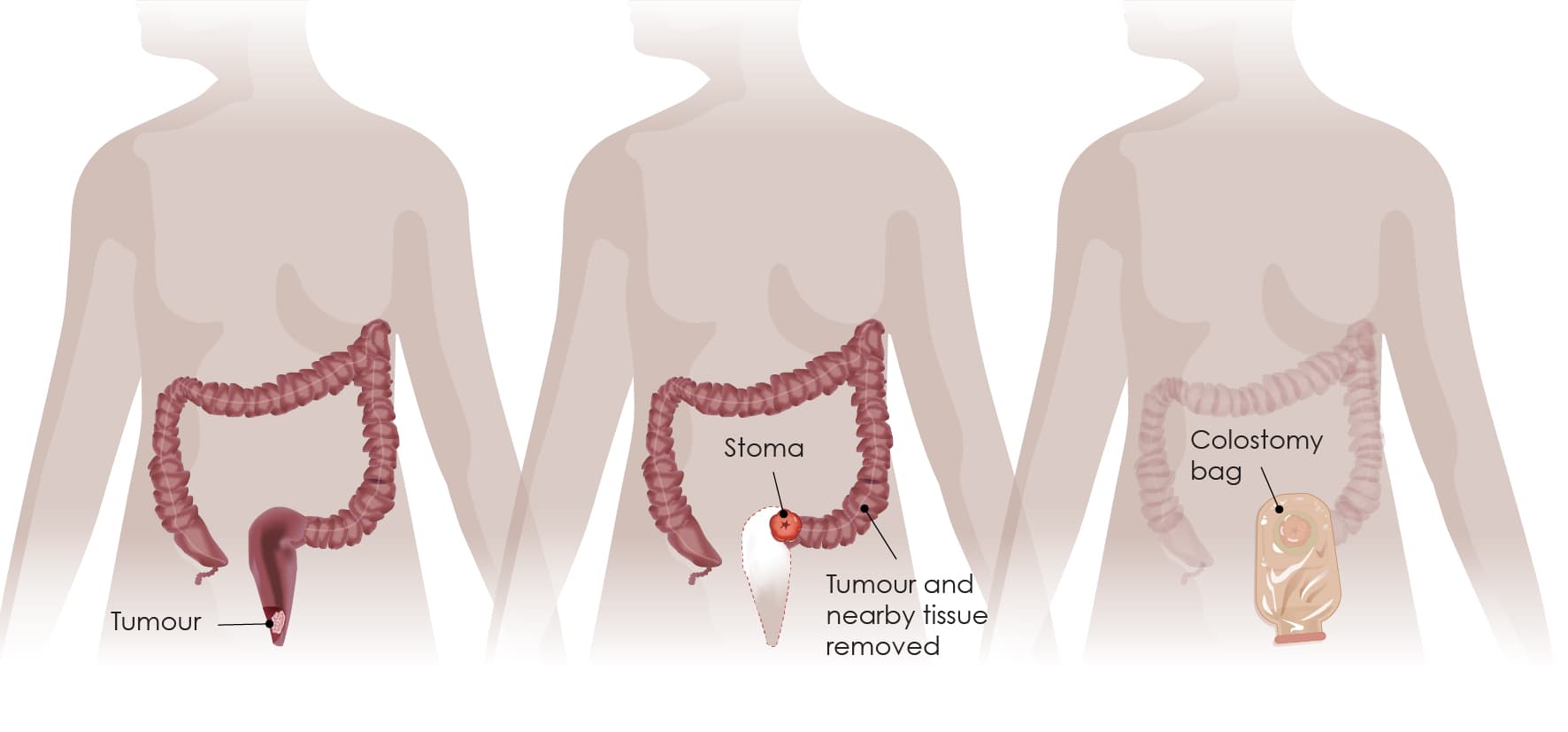
- Low anterior resection (LAR)
- Some stage I rectal cancers and stage II or III cancers in the upper part of the rectum (close to where it connects with the colon) can be removed by low anterior resection (LAR). During the operation, the part of the rectum containing the tumour is removed with the surrounding lymph nodes. The colon is then attached to the remaining part of the rectum.
- Some patients may need to undergo colostomy, resulting in a stoma in the abdomen (see above).
An illustration of low anterior resection with colostomy. The first image (left panel) shows the rectum with the tumour. The second image (middle panel) shows the rectum and colon during surgery – the tumour has been removed and a stoma has been created. The third image (right panel) shows a colostomy or stoma bag attached to the stoma.
- Abdominoperineal resection (APR)
- This type of surgery can be used to treat some stage I and II cancers in the lower part of the rectum when the tumour is growing into the sphincter muscle or the nearby muscles that help control urine flow.
- This operation is more invasive than a low anterior resection because the anus is removed, and a permanent colostomy is created to allow stool to leave the body.
After surgery
Following surgery, no other treatment may be required. However, to reduce the chances of any cancer cells remaining in the area, after surgery the patient may undergo chemotherapy, known as ‘adjuvant chemotherapy’.
Recent research has uncovered that a specific combination of molecules (biomarkers) found in T cells, a type of cells of the immune system, may predict how likely it is that an early-stage colorectal cancer patient relapses (the cancer returns) after surgery. In case the test indicates a high likelihood of relapse, then the patient should undergo adjuvant chemotherapy to reduce this risk. However, if the test indicates a low likelihood of relapse, then chemotherapy may be avoided. That way the patient will not experience the side effects of chemotherapy.
The procedure for the test is fairly simple. With the patient’s consent, tumour tissue is sent to the pathology laboratory. The turnaround time is short, and the oncologist is notified quickly of the result to allow prompt initiation of chemotherapy, if seen appropriate.
We encourage patients to participate in the shared decision-making process with their physician to understand how their own immune system can help their treatment in this highly innovative framework of personalised medicine. With such a refinement in diagnostic information, over-treatment or under-treatment with adjuvant chemotherapy is prevented. However, testing for these specific biomarkers is not currently reimbursed by the national health systems and the patient would need to cover the costs for this screening.