New Study – Cost of All Digestive Cancers in Europe Exceeds 40 Billion Euro
New study calculates total costs – lives can be saved, and money can be saved
For the first time ever, the total cost of all digestive cancers across Europe has been evaluated by type of digestive cancer, by type of cost and by country. Digestive Cancers Europe, the umbrella organisation of all national associations of patients with digestive cancer, commissioned this study to the Swedish Institute for Health Economics (IHE) in order to enable informed policy choices about investments in the prevention and treatment of digestive cancer patients.
Every year, more than 900,000 citizens in Europe receive a diagnosis of oesophageal, gastric, colorectal, pancreatic, liver cancer or other rare cancers of the digestive system. Despite the fact that most digestive cancers are preventable, 600,000 patients die every year.
The Institute of Health Economics analysed the complete costs of each digestive cancer by country. Their evaluation included:
- The direct health costs, such as hospitalisation, surgery, imaging, chemotherapy
- The costs of informal care
- The indirect health costs caused by premature mortality and morbidity
IHE carried out this study across 31 countries: the EU-27 member states, Iceland, Norway, Switzerland and the UK for the year 2018.
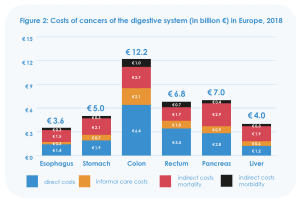
For the selected countries, digestive cancer costs amounted to 39 billion euro in 2018, of which around 17 billion euro account for direct cost and 22 billion euro for indirect costs and informal care costs. This is equivalent to 19% of total cancer costs and is the case for most European countries. The total absolute costs of a cancer type are mainly determined by the number of patients suffering from the disease. The total cost of all digestive cancers in the whole of Europe will be significantly more than 40 billion euro.
The graph below shows that the actual number of patients is the main driver of the costs, but also that digestive cancer types with a high mortality rate result in high cost of premature mortality.
Stefan Gijssels, CEO of Digestive Cancers Europe comments: “It is surprising to see that despite the cost of healthcare, no systematic analyses are made by governments to evaluate the total cost by disease. This appears to be the very first step that is needed to ensure that the right health policy decisions are made. Patients are treated suboptimally in every country in Europe. Many advances can be made based on the application of best practices. Lives and money can be saved. At a time where the European Commission is developing it’s “Beating Cancer Plan”, we hope that our report can be a debate starter to make more rational decisions on quality cancer care in the Member States”.
Thomas Hofmarcher, lead author of the study report: “The basis of evidence-based policy making is the availability of comprehensive and up-to-date data. This report fills an important void and provides the first-ever pan-European estimates of the total costs of digestive cancers. It is striking to see that more than half of the costs occur outside the healthcare system. Policy makers need to realise that decisions on investments in cancer care always also affect costs outside the healthcare system. This calls for broader perspective in future decision-making on the allocation of healthcare resources to cancer care.”
Based on the health economic evidence put forward in this study, Digestive Cancers Europe has developed the following recommendations on how to best manage digestive cancers in Europe. These can also be found in our accompanying White Paper ‘The Economic Burden of Digestive Cancers in Europe‘:
- To develop cancer-specific policies that take into consideration:
- The full patient journey, from prevention, early detection, screening and timely intervention and treatment, to follow-up, return to work or end of life
- Informal care and indirect costs, moving away from a silo-budgeting mentality
- The need to harmonise the patient referral process to ensure patients are systematically directed to a cancer expert centre that meets the European Cancer Organisation’s Essential Requirements of Quality Cancer Care.[1]
- A 360 degrees – multidisciplinary approach to cancer management should be a priority, with a collaboration among all partners: screening agency, hospitals, laboratories, diagnostic companies, general practitioners, primary care professionals, medical experts and patient organisations
- The need to reduce the approval times for new cancer therapies in national pricing & reimbursement systems as these vary importantly from one country to another.[2]
- To empower cancer-specific patient organisations with the double objective of offering patient support and education as well as leading multi-stakeholder design of optimal patient pathway
- To gather data and develop further research for each cancer type at country level in order to understand the full burden of each cancer costs and better adapt future cancer policies
The full report can be downloaded from the website of the Institute of Health Economics or the website of Digestive Cancers Europe.
For more information please contact us.
References
[1] https://www.europeancancer.org/2-content/8-erqcc
[2] EFPIA Patient W.A.I.T. Indicator 2018 (https://www.efpia.eu/media/412747/efpia-patient-wait-indicator-study-2018-results-030419.pdf) and EFPIA-sponsored Vintura report on Improving Time To Patient Access To Innovative Oncology Therapies In Europe: Every Day Counts (https://www.efpia.eu/media/554647/every-day-counts-improving-time-to-patient-access-to-innovative-oncology-therapies-in-europe.pdf).
Author: